Healthcare Affordability, Innovation, and Health Plans
December 8, 2025
By Linda Leigh Brock, Vice President, Product Management
As virtually everyone in healthcare knows all too well, we are in the midst of an affordability crisis that is adversely impacting every stakeholder—health plans, physicians and clinicians, hospitals, employers, and patients.
For health plans in particular, the affordability crisis is an immediate call-to-action to go beyond narrow approaches to deliver higher value products and better experiences, now. At NASCO, we are enabling our health plan customers with a portfolio of products and services that drive affordability.
Employers Facing Highest Health Cost Increase in 15 Years
In a previous blog about healthcare affordability and innovation, NASCO President and CEO Lori Logan wrote about health costs increasing every year. As the American Medical Association shared,
“Health spending in the U.S. increased by 7.5 percent in 2023 to $4.9 trillion or $14,570 per capita. This growth rate is significantly higher than the 4.6 percent rise in 2022, and apart from the 10.4 percent rise in 2020 due to the COVID-19 pandemic, it is the highest growth rate observed since 2003.”
In 2025, the average family health insurance premium is $26,993, up six percent since 2024.
The predictions for 2026 are even more dire as employers are expected to face the highest health cost increase in 15 years and, on average, ACA Marketplace insurers are raising premiums by ~26 percent.*
The Affordability Crisis:
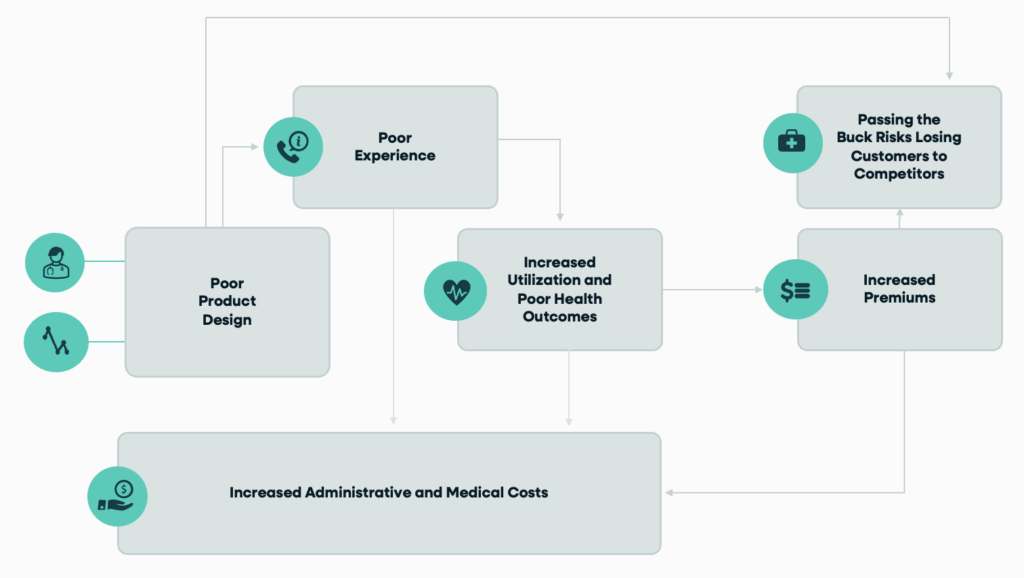
To mitigate the healthcare affordability crisis, health plans must deliver higher value products and better experiences.
In October, we introduced NASCO Evolve to solve health plans’ biggest barrier to affordability: accurately adjudicating payments in a growing mixed-model environment of claims and non-claim transactions. NASCO Evolve enables health plans to operationalize affordability across the alternative payment model (APM) life cycle—from informing provider contracting to understanding cost and quality performance and determining settlement based on results—empowering health plans to understand the total cost of care faster.
Today, I want to share another important way NASCO is driving affordability for health plans, and that is, enabling them to compete with alternative health plans (AHPs) and similar copay plans based on product innovation at scale.
The Challenge and the Opportunity of Alternative Health Plans (AHPs)
Allow me to first set the stage.
I believe the increasing interest in AHPs poses a market challenge—and an opportunity—to Blue plans. The challenge is to compete on both innovation and cost, effectively neutralizing employer interest in stitching together multiple, specialized health solutions all promising improved care outcomes and lower costs. The opportunity is to retain and grow a plan’s commercial business with one experience and brand and a full suite of innovative products to address the unique needs of each employer group customer. That’s what truly transformational and scalable product innovation is and does.
Employer Interest in AHPs is Growing
In March and April 2024, Mercer surveyed nearly 700 organizations for its Survey on Health and Benefits Strategies for 2025. Among employer priorities is an “increasing interest in offering a medical plan option that is focused on steering employees to quality, cost-efficient health providers—and potentially offers members more affordable coverage.” More than one-third of large employers (36 percent) said their organizations were utilizing high performance networks or other AHPs in 2024, and another 29 percent said it was a near-term consideration.
High-performance networks, alternative health plans and other network optimization offerings are gaining traction:
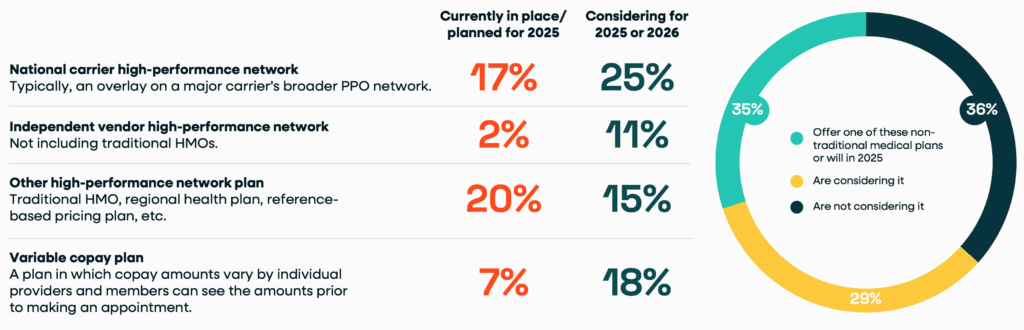
Employer interest in AHPs is growing. The full Mercer report can be downloaded here.
Healthcare Affordability and the Three Trends Fueling Employer Interest in AHPs
There are three key market trends driving employer interest in and the adoption of AHPs:
- Employers and members are demanding simplicity and price transparency in the search for low-cost high-quality care. In turn, employers are opting for simplified health plan models, steerage, price certainty, and member financing options, spurring differentiation of AHPs.
- Employers are prioritizing high performing networks/risk-based, carve-outs, specialty pharmacy, product packaging, and more for improved affordability. They are turning to non-traditional health plans, high quality networks, performance insights, and improved pricing models with integrated prevention and treatment, forcing payers to partner with third party administrators (TPAs).
- Employer and consumer year-over-year cost increases are increasing interest in financial flexibility, predictability, and containment options over traditional methods. The growing adoption of AHPs, Individual Coverage Health Reimbursement Arrangements (ICHRAs), self-funded and level funding arrangements, and the like comes with the goals of predictability and lowering cost, highlighting the need for a unified employer experience.
How NASCO Helps Health Plans Compete with AHPs and Drive Healthcare Affordability
Health plans are all seeking ways to provide affordable options and need strong partners with the right solutions to get there. In lieu of AHPs—which are no longer limited to select large employer group segments—payers need a holistic strategy to support all employer groups.
The key elements of a minimum viable product (MVP) solution for a differentiated health plan are:
- Simplified Offering: Enable the selection of high-value provider services with simplified and calculated copay upfront.
- Network Design: Use of national and local provider data to enrich and create network options that allow the health plan to configure networks and enrich data with insights from their local markets
- Benefit Design: Provide a benefit catalog and service bundle templates with plan defined products, service bundles, and copay logic.
- Member Experience: Provide digital tool options for care finder with navigation, payment clarity, potential member financing integration, and member, claims, and benefit accumulation as part of member liability estimator (MLE)—all with a plan-defined experience, brand, and service integration.
- Product Packaging: Membership and billing management with benefit linkage and integration to buy-ups and other charges that leverage plan underwriting as well as rates and fees determination. Leverageable product capabilities to offer flexible billing terms, level billing, settlement automation, and integrated stop loss solutions so health plans can better meet the needs and expectations of employers and members.
Even more exciting is our collaboration with health plans to move beyond the MVP and parity to support continuous product innovation at scale. Our approach equips plans to succeed in new markets and retain current customers with improved affordability.
NASCO’s strategic objectives for enabling health plans to define market-leading solutions are to:
- Differentiate our health plan customers in the AHP market for strategic accounts.
- Increase employer sponsor satisfaction and retention by lowering the total cost of care.
- Improve member outcomes through steering towards higher value providers.
At NASCO, we are committed to partnering with health plans to meet their affordability and innovation challenges by empowering organizations with the tools needed to efficiently and effectively design new product offerings that satisfy market demands. We bring the holistic perspective that enables health plans to understand and retain their entire book of employer business.
Coming soon is the next blog in our series about how NASCO is driving healthcare affordability. Click here to read the first blog in the series!
*This information is current as of December 3, 2025.
